In 1902, the first electrocardiograph device used a galvanometer made of string to measure the heart's electrical activity. Then, in the 1950s a 12-lead electrocardiogram became available to detect arrhythmias and heart diseases. The electrocardiogram soon became essential for health care providers as a non-invasive, affordable, tool that provided information quickly about the status of a patient's heart.
ECG in Practice: Q&A With Galina Roofener
Today, electrocardiogram devices (ECG or EKG) are mobile and available for personal use to record the timing and strength of heartbeats via the electrical impulses that contract the heart. East Asian medicine practitioner Galina Roofener, Dipl. OM (NCCAOM), LAc, uses a mobile ECG to evaluate the Chinese medical pulse quality remotely. I had the opportunity to familiarize myself with Galina's technique while editing her new book on the subject. She joins me in an interview here to share how she is using an ECG in her clinical practice.
Q: Galina, I'm excited to sit with you once again and talk about big new ideas. This time, let's cover how you use a mobile ECG device to detect a traditional Chinese medical (TCM) pulse pattern. Can you tell our readers what prompted you to look at an ECG as a tool for collecting the TCM pulse?
A: Four years ago, the administration at the hospital I am employed by approached me with possibilities to provide Traditional Chinese Herbal Medicine consults via telemedicine appointments. As I considered the methods for delivering this service, I recognized the most significant challenges I would encounter were to find ways to produce objective data, such as tongue and pulse, from patient visits virtually. My colleague, Susan Veleber, and I had to create clear directions to teach our patients how to photograph their tongues with consistency accurately.
Once this was achieved, the next challenge was to tackle the reading of the pulse. I considered many technological pulse-taking devices. After compiling my research, I determined that the best solution would be to use a mobile electrocardiogram (ECG) device. This was primarily because of its widespread acceptance in broader medical systems.
The single-lead ECG mobile device that I recommend for my patients is widely available, affordable, FDA approved, HIPAA compliant, and records a standard ECG a patient can share with their MD. Eureka! Throughout the past year, I have taken an ECG on every patient. There is definitely a relationship between ECG readings and the TCM pulse pattern!
Q: Some practitioners have undertaken in-depth study of TCM pulse patterns, and some practitioners do not use pulse diagnostics at all to determine a TCM-differentiated pattern for a patient. Those who swear by the findings of the pulse claim it is the primary reflection of qi and blood throughout the body that a practitioner can measure. However, with varied methods, there may be discrepancies in how the pulse is discerned from practitioner to practitioner.
A drawback of pulse diagnosis is in the subjective nature of the traditional reading method. One patient seen by three practitioners may have three different ways of describing the TCM pulse pattern. Lack of consistency can lead to scrutiny in a Western medical integrative setting. How do you manage pulse reading mastery and consistency in your practice?
A: In modern times, the majority of us do not have an option to apprentice a TCM master for 10 years. At best, during clinical rounds in the college clinic, we will palpate pulses of about a hundred patients. Hence, [it is ]no wonder that three different practitioners will read pulse differently. Li Shi Zhen described 29 pulses in his book Pulse Diagnosis, Paradigm Press; 1 edition (Feb. 8, 1993). The WHO International Standard Terminologies on Traditional Medicine in the Western Pacific Region, World Health Organization (WHO)(2007), [which] is a basis for terminology to be used in future ICD-11, has 48 TCM pulse descriptions. Current U.S. TCM practitioners most commonly use 14 pulses.
When I read the 48 pulses presented by the WHO, I thought, "I need to go back to school!" Then I realized the beauty was that regardless of language or translations, these definitions standardize terms, allowing everyone to communicate [and] avoiding language translation discrepancies.
Q: Can you share examples of pulse descriptions?
A: Yes, here are descriptions of both a deep and a wiry pulse with the WHO code and name:
WHO code |
WHO name |
WHO description |
Current US name |
| 2.4.30 | sunken pulse | a deeply located pulse which can only be felt when pressing hard, also called deep pulse | deep pulse |
| 2.4.41 | string-like pulse | a straight, long and taut pulse, like a musical string to the touch | wiry pulse |
Q: The chart you share illustrates a way to organize both descriptive elements of the palpatory findings with codes and specific terms. For many practitioners engaged in research or who wish/need to maintain accurate clinical records, having specific codes and terms is a benefit. Process and methods of entering data points in clinical records need to be reproducible. The ability to show changes in the pulse is a help with the increasing request from patients, insurance companies, and medical peers for practitioners to illustrate outcomes. The ECG report offers a visual graph that can also become a permanent part of a patient record. Can you share with us how you record the findings of an ECG?
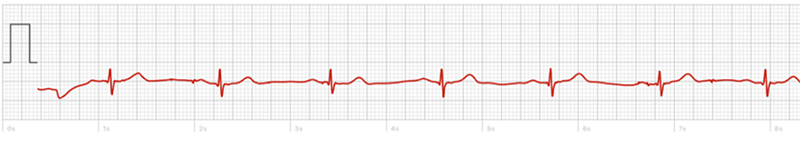
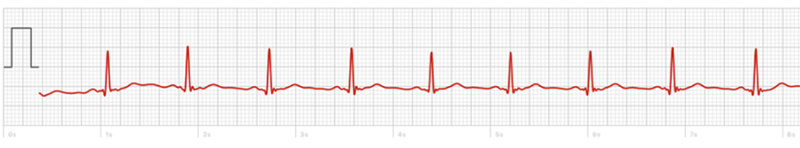
A: Absolutely. Here are two examples. (More examples and the way to interpret an ECG in TCM terms are available in my textbook.)
Example #1: Slow (54 beats per minute), vacuous, sunken, regular, thin pulse.
Example #2: Moderate (71 beats per minute), slightly uneven, rootless, regular, string-like pulse.
Clinical Takeaway
The ECG reports can tell a lot about the patient. The devices are designed to report from a Western medical lens. If the patient's heart rate is within a measurable range, the mobile ECG devices can evaluate the upper and lower chamber heart contractions to detect sinus rhythm patterns (between 50-100 BPM) and irregular rhythm patterns (between 50 and 120 BPM), such as atrial fibrillation. Low heart rate numbers below 50 BPM and high numbers over 120 BPM can indicate a need for further testing at a medical facility. The devices do not detect a heart attack, blood clots, stroke, high blood pressure, high cholesterol, or heart conditions.
The use of diagnostic tools must be understood by both the patient and the practitioner as ways of better understanding subtle diagnostic aspects of the cardiovascular system and in the context of this conversation, the traditional Chinese medical pulse pattern.
The ECG reading is not a replacement for a Western medical examination. TCM practitioners must be aware of urgent cases that need an immediate referral and remain within their scope of practice when implementing new medical devices.
Consistent terminology and record- keeping are critical for TCM practitioners to work together and with medical peers from other systems. Integrative TCM practitioners who include objective data such as an ECG-based TCM pulse and consistent terminology in patient reports may gain greater confidence from Western medical peers and greater ability to provide integrative care.
If you need support in learning these techniques, you can find a wealth of information in Galina's book, Modern Pulse Diagnosis: Mobile ECG and at her website, www.AsianTherapies.org/books.




