Unfortunately, "long COVID" or "long haulers" are already or may soon become part of your practice, but understanding how to support patients on a mitochondrial level will go a long way toward improving outcomes for this stubborn condition.
The Connection
Mitochondria are organelles that convert fat, protein and carbohydrates in the food we eat into energy in all of our cells, and produce 90-95 percent of the body's total energy.
Some of the common symptoms of long COVID include fatigue, brain fog, pain, shortness of breath and dysrhythmias, and sleep issues; all of which are symptoms of myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS).
Scientists agree that chronic fatigue can be driven by viruses that cause mitochondrial dysregulation such as cytomegalovirus (CMV), Epstein-Barr virus (EBV), herpes simplex virus type 1 (HSV-1), and hepatitis virus (HCV). Similarly, infections with SARS-CoV-2 tend to upregulate carbon metabolism, decreasing oxidative phosphorylation, increasing glycolysis and decreasing mitochondrial energy yield.
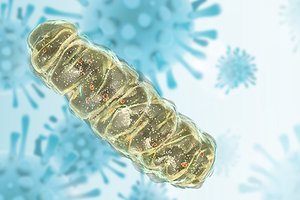 The cytokine storm (aka, hyperinflammation) is a well-known pathology related to COVID-19 and is triggered by a huge increase in reactive oxygen species (ROS). Through complex biochemistry involving that inflammatory cascade, the SARS-COV-2 infection alters mitochondrial physiology.
The cytokine storm (aka, hyperinflammation) is a well-known pathology related to COVID-19 and is triggered by a huge increase in reactive oxygen species (ROS). Through complex biochemistry involving that inflammatory cascade, the SARS-COV-2 infection alters mitochondrial physiology.
A Therapeutic Regimen
Understanding this and other aspects of the effect of the virus on mitochondrial function, we can recommend some supplements that can re-establish optimal cellular energy production and reduce the symptoms associated with long COVID.
For instance, calcium is an important electrolyte that's involved with mitochondrial dynamics and helps control ATP production, among other things. COVID is known to reduce calcium levels, promoting ROS formation leading to an inflammatory cascade. Supplementing with calcium, magnesium and vitamin D3 would be helpful to support mitochondrial function.
Furthermore, since free-radical and oxidative stress are involved in mitochondrial dysfunction, supplementing with powerful antioxidants such as ubiquinol (reduced CoQ10), vitamin E and glutathione can offer symptomatic relief.
CoQ10 happens to be the only lipid-soluble antioxidant synthesized in the human body, allowing it to move freely within the phospholipid bilayer. Roughly half of all the CoQ10 in our body is found in the mitochondrial membranes, and the highest concentrations found elsewhere are located in highly metabolic tissues such as the liver, heart and skeletal muscle. (Keep in mind that anyone on statin medications should automatically be supplementing CoQ10).
D-ribose, which is involved with ATP production, is known to reduce fatigue in both CFS and fibromyalgia patients. A powder form is recommended over capsules based on the daily dosage of 15 g, split into three doses.
Alphalipoic acid (ALA), which is commonly used to combat neuropathies, may also play a part in the treatment of long COVID. ALA is part of the Krebs cycle and regulates nucleic acid synthesis and ATP production. It also acts as a free-radical scavenger that may interfere with viral progression. Oral supplementation is safe and well-tolerated, and has been well-studied for its antioxidant and immunomodulatory actions.
Fermented wheat-germ extract is a common nootropic used to decelerate aging, and helps restore mitochondrial function. It's currently the focus of research as an anti-cytokine-storm and anti-cancer drug. The benefits of being in nature and exposure to sunlight are well-documented (see my previous column, "Shedding Light on the Benefits of Heliotherapy"), where sun exposure was used to treat tuberculosis patients in the late 1800s.
Near-infrared light from the sun (or heat from a fireplace) is beneficial and can easily pass through clothing (reducing cytokines), and is strongly recommended for those suffering from long COVID. Wintertime limits sun exposure, so encourage your patients to get outside anyway. Studies relating to COVID morbidity demonstrate poorer outcomes for those who spend a majority of their time indoors.
Serum concentrations of ascorbate (vitamin C) in COVID-19 patients have been found to be significantly lower than healthy controls, and plasma ascorbate levels below 11.4 µM are associated with a higher risk of death and longer hospitalization rates.
Buffered C supplementation would be appropriate to promote improved immune response to the infection, reducing inflammation (lowering IL-6 levels), increasing peripheral capillary oxygen saturation (limiting the need for forced ventilation), improving biosynthesis of collagen, and reducing oxidative stress as an electron donor.
You Can Make a Difference
Understanding the underlying mitochondrial dysfunction associated with long COVID patients can assist you in bringing them back to homeostasis and relieving their symptoms of fatigue, brain fog, shortness of breath and insomnia.
Resources
- Aguida B, et al. Infrared light therapy relieves TLR-4 dependent hyper-inflammation of the type induced by COVID-19. Commun Integr Biol, 2021 Sep 15;14(1):200-211.
- Alfarouk KO, et al. Of mitochondrion and COVID-19. J Enzyme Inhib Med Chem, 2021 Dec;36(1):1258-1267.
- Barletta MA, et al. Coenzyme Q10�+�alpha lipoic acid for chronic COVID syndrome. Clin Exp Med, 2022 Aug 22:1-12.
- Bencze G, et al. Mito-oncology agent: fermented extract suppresses the Warburg effect, restores oxidative mitochondrial activity, and inhibits in vivo tumor growth. Sci Rep, 2020;10:14174.
- Contreras L, et al. Mitochondria: the calcium connection. Biochim Biophys Acta, 2010;1797:607-18.
- Khan M, et al. Mitochondrial dynamics and viral infections: a close nexus. Biochim Biophys Acta, 2015;1853:2822-33.
- Mehmel M, et al. Nicotinamide riboside - the current state of research and therapeutic uses. Nutrients, 2020 May 31;12(6):1616.
- Missailidis D, et al. An isolated complex V inefficiency and dysregulated mitochondrial function in immortalized lymphocytes from ME/CFS patients. Int J Mol Sci, 2020;21:1074.
- Reshi L, et al. Modulation of Mitochondria During Viral Infections. In: Taskin E, Guven C, eds. Mitochondrial Diseases. London: InTech, 2018: pp. 11.
- Saleh J, et al. Mitochondria and microbiota dysfunction in COVID-19 pathogenesis. Mitochondrion, 2020;54:1-7.
- Singh KK, et al. Decoding sars-cov-2 hijacking of host mitochondria in covid-19 pathogenesis. Am J Physiol Cell Physiol, 2020;319:C258-C267.
- Sinnberg T, et ak. Vitamin C deficiency in blood samples of COVID-19 patients. Antioxidants, 2022;11(8):1580.
- Teitelbaum JE, et al. The use of D-ribose in chronic fatigue syndrome and fibromyalgia: a pilot study. J Altern Complement Med, 2006 Nov;12(9):857-62.
- Tiku V, et al. Mitochondrial functions in infection and immunity. Trends Cell Biol, 2020;30:263-75.
- Tomas C, et al. Cellular bioenergetics is impaired in patients with chronic fatigue syndrome. PloS One, 2017;12:1-16.
- Zhong M, et al. A randomized, single-blind, group sequential, active-controlled study to evaluate the clinical efficacy and safety of a-lipoic acid for critically ill patients with coronavirus disease 2019 (COVID-19). medRxiv, 2020:2020.04.15.20066266.
Click here for more information about Bill Reddy, LAc, Dipl. Ac..




